October 20-26 was National Respiratory Care Week, and we just want to take a moment to remind you how your cardiovascular health and respiratory health go hand-in-hand.
The heart and the lungs work together to make sure the blood in your body is oxygenated efficiently. The right side of the heart takes the blood that’s lacking oxygen from the body, and pumps it directly into the lungs to be reoxygenated. Once the blood is full of oxygen, the left side of the heart pumps the blood from your lungs and back through the body, so it can get the oxygen it needs.
Because the heart and lungs work in tandem, that means that circulo-respiratory problems such as shortness of breath, chest pain, near fainting, or fatigue can be linked to either the heart, the lungs or both!
This doesn’t mean that every breathing problem is linked to the heart. Being out of shape, being congested, or having asthma are symptoms that are not linked to heart health. However, you should still consult your doctor with any of those symptoms to rule out a bigger and more serious issue—heart failure.
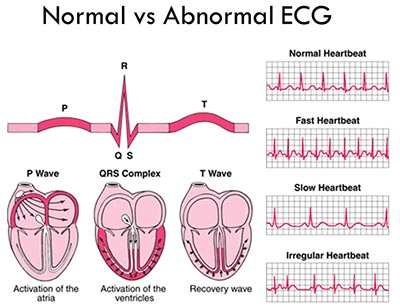
Heart failure means that your heart is weak, and a few heart problems can occur when you’re in heart failure such as tachycardia, pulmonary edema, or cardiomyopathy.
Tachycardia is a fast heart rate, which can lead to shortness of breath. Pulmonary edema is a condition where the heart is too weak to pump blood out of the lungs, so pressure builds in the heart, and fluid builds up in the lungs, which then causes breathing problems. Cardiomyopathy is a serious heart condition that inhibits blood from efficiently being pumped throughout the body. Cardiomyopathy can be linked to heart attacks, excess weight, diabetes or high blood pressure. With cardiomyopathy, breathing issues occur because the blood isn’t being pumped properly, so it can’t be fully oxygenated, which leads to a whirlwind of problems.
If you are experiencing any of these circulo-respiratory problems, please schedule an appointment today. Take care of your respiratory health, and take care of your heart! Oh, and happy belated Respiratory Care Week from Cardiovascular Institute of the Shoals!



 properties called lycopene.
properties called lycopene.
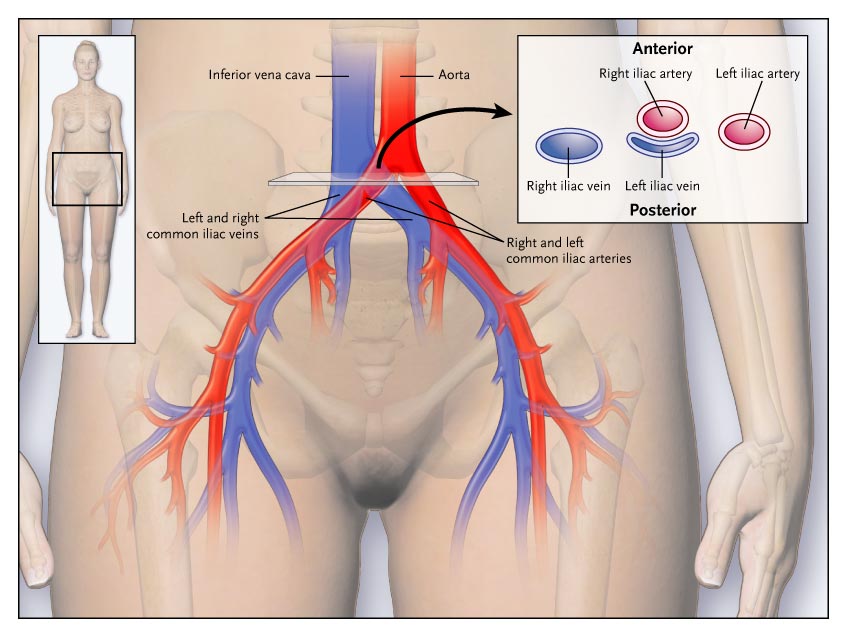
 Healing, wounds, and fighting infections both require a healthy blood supply therefore injuries must be monitored carefully in patients who are at the risk for PAD. In extreme cases, when you have a wound that becomes neglected, the soft tissue surrounding the wound can die and require amputation. Painful dry, gray, or black sores could be signs of either severe Peripheral Artery Disease or another condition that should be examined by a doctor as soon as possible.
Healing, wounds, and fighting infections both require a healthy blood supply therefore injuries must be monitored carefully in patients who are at the risk for PAD. In extreme cases, when you have a wound that becomes neglected, the soft tissue surrounding the wound can die and require amputation. Painful dry, gray, or black sores could be signs of either severe Peripheral Artery Disease or another condition that should be examined by a doctor as soon as possible.